Retinal Detachment
What is Retinal Detachment?
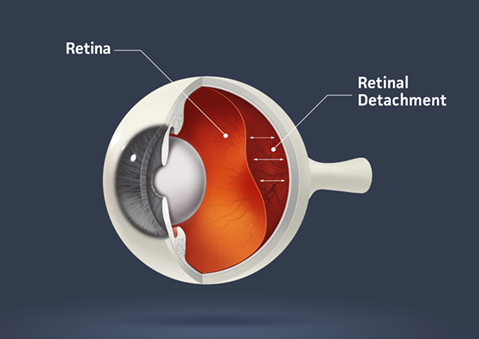
The retina acts like film in a camera, capturing images and sending them to your brain through the optic nerve. When the retina detaches, it separates from the back wall of the eye, disrupting its ability to function correctly. It’s essential to know that retinal detachment is a severe eye problem that needs immediate attention from an eye doctor, also known as an ophthalmologist.
What are the symptoms of Retinal Detachment?
Recognizing the signs of retinal detachment is crucial for getting timely treatment. Some common symptoms to watch out for include:
- Floaters: Seeing tiny specks or spots drifting in your vision, which may look like little bugs or cobwebs.
- Flashes of Light: Brief flashes or sudden bursts of light in your vision, even when you’re in a dark room.
- Blurred Vision: Experiencing blurred or reduced vision, as if a curtain or shadow is moving across your eye.
- Loss of Peripheral Vision: Noticing a loss of side or peripheral vision.
If you ever notice these symptoms, it’s essential to tell an adult or your parents immediately. Remember, early detection is crucial for effective treatment.
What are the treatment options for Retinal Detachment?
Once diagnosed, there are a few methods doctors might use to treat retinal detachment:
- Surgery: The most common treatment involves surgery to repair the detached retina. There are various surgical techniques, but the primary goal is to reattach the retina to its proper place. Sometimes, tiny air or gas bubbles may be used to push the retina back into position.
- Laser Therapy or Cryopexy: In certain cases, doctors may use laser therapy or freezing (cryopexy) to repair small retinal detachments by sealing the tears or holes in the retina.
- Medication: While medication alone cannot reattach the retina, eye drops or injections might be used alongside surgery to prevent infections or reduce inflammation.
Remember, the type of treatment needed depends on the severity of the detachment and other individual factors. Your doctor will decide the best course of action.
Macular Degeneration
What is Age-Related Macular Degeneration (ARMD or AMD)?

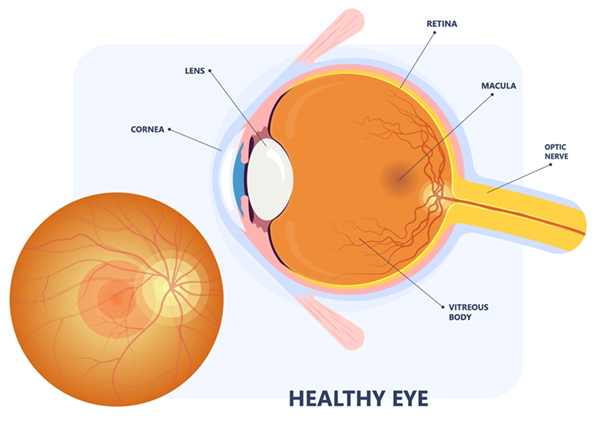
AMD is the most common cause of vision loss in individuals over age of 50. The name of the condition is derived from its cause which is damage to the macula. Macula is the most sensitive central part of the retina responsible for central vision and is required for clarity of central part of the visual field. Macula degeneration progresses at different rates in different patients and has a strong genetic component where it runs in families. While even in end stage AMD patients are not completely blind, retaining peripheral vision, normal everyday activities like reading and driving become increasingly difficult.
There are two main categories of macular degeneration: Dry (non-exudative) and wet (exudative or neovascular) AMD.
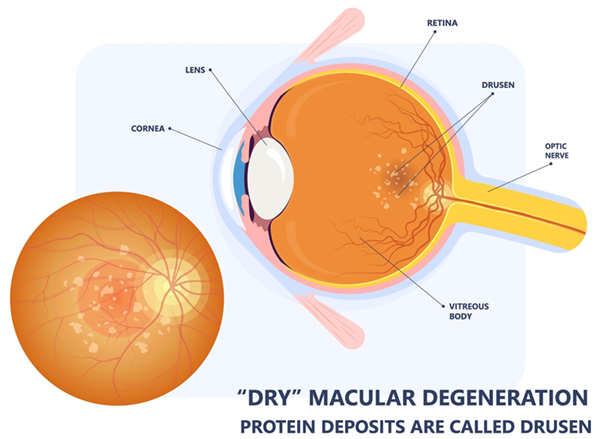
What are 3 stages of dry ARMD?
- Early stage: small/medium yellow deposits underneath the retina are present and there are possible pigmentary changes in the macula. These patient usually don’t experience any visual symptoms.
- Intermediate stage: Medium/large drusen are observed and pigmentary changes. Small gaps in vision and distortion may be experienced but no significant visual loss.
- Advanced Stage: There is progressive atrophy in the macula often with missing spots of tissue called geographic atrophy (GA). During this stage patients experience significant vision loss.
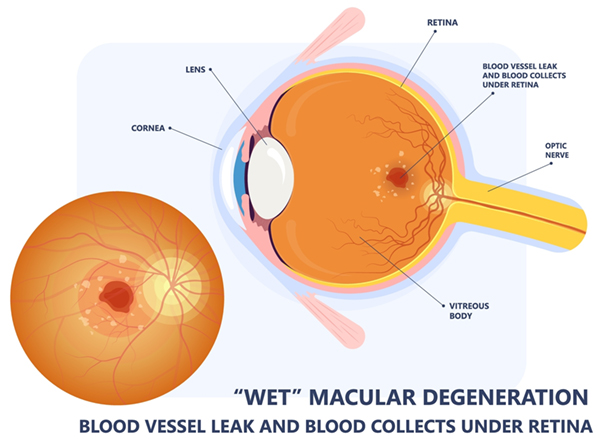
What is wet AMD?
Onset is usually more rapid than dry with newly developed abnormal blood vessels underneath the retina that may leak fluid or blood. Visual symptoms are much more rapid but patients may not notice if only one eye is effected (especially if it is a nondominant eye). If not treated wet AMD can cause permanent visual loss rapidly.
What are risk factors for AMD?
- Age > 50
- Poor diet
- Smoking
- Excessive exposure to sunlight
- Genetic predisposition with close family member affected
- Females
- Light skin
What are the symptoms of AMD?
- Wavy lines
- Gradual lessening of color perception
- Distorted or blurry vision
- Dimming of vision and need for more light to see
- Missing spots in the center of the visual field
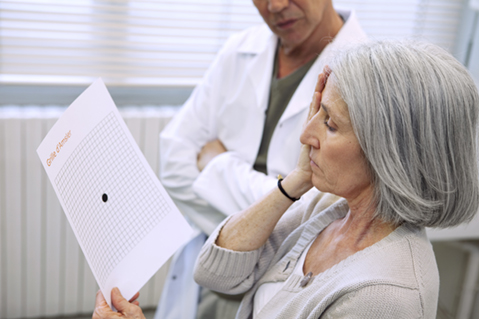
How is AMD diagnosed?
- Visual acuity test
- Dilated examination of the back of the eye
- Amsler grid test of central vision
- Optical coherence tomography (OCT)
- Fluorescein angiogram (sometimes) – dye test of the blood vessels in the back of the eye
What is the treatment of AMD?
While there is no cure for AMD, many patients have been helped greatly by recent innovations in treatment. Regular examinations to facilitate early detection of AMD and check for progression are essential. This is because most therapies work best when started in early stages of AMD.
Recommended treatments for AMD may include one or more of the following, each of these approaches controlling AMD in different ways.
- Vitamins and minerals in a supplement called AREDS2 which was determined and recommended by retina specialists based on a large rigorous clinical trial. Patients should look specifically for the vitamins that say AREDS2 formula on the bottle.
- For wet AMD injections of anti-VEGF (Vascular Endothelial Growth Factor) with options that include Avastin, Lucentis, Eylea, Cimerli, Byooviz, Vabysmo
- For advanced dry AMD there are recent therapeutics that have been approved and constitute intravitreal injections by the name Izervay and Syfovre – these have been shown to delay progression of Geographic Atrophy
- Laser – less common but occasionally a good option for treatment of AMD
- End stage AMD can be treated with low vision devices and even implantable miniature telescope (IMT) in order to reduce the size of the blind spot.
There have been many important development in the treatment of AMD in the past two decades and with todays treatment options doctors are able to preserve patients vision in majority of cases.
The Valeda Light System for Dry AMD
The Valeda Light Delivery System offers a new approach for treating dry age-related macular degeneration. This is the first FDA authorized device for dry AMD and uses specific yellow, red, and near-infrared light to target the retina, helping to restore damaged eye cells.
During treatment, patients simply sit comfortably while the system delivers therapeutic light in a quick, painless session. The Valeda system is especially valuable for people with dry AMD who still have reasonable vision but show signs of retinal damage and drusen deposits.
Treated patients are typically able to read an additional line on eye charts after two years of therapy compared to those without treatment. This innovative light therapy provides a non-invasive option for potentially slowing vision loss and improving sight in a condition that has previously had limited treatment alternatives.
Flashes & Floaters
What Are Floaters?

Imagine tiny particles floating inside a snow globe; that’s somewhat like what floaters are in your eyes. They’re small, shadowy shapes that drift around when you move your eyes. These floaters are made up of tiny bits of a substance called vitreous gel that fills the inside of your eye. When these bits cast shadows on your retina (the part of your eye that helps you see), you notice them as floaters.
What Are Flashes of Light?
Flashes of light are like tiny sparks or lightning bolts that suddenly appear in your vision. They might look like bright streaks or stars. These flashes happen when the vitreous gel inside your eye pulls or tugs on your retina. When this occurs, it sends signals to your brain, making you see these bursts of light.
When Should You Worry About Floaters and Flashes?
Most of the time, floaters and occasional flashes are normal and not a cause for concern. However, there are instances when you should tell an adult or an eye doctor:
- Sudden Increase in Floaters: If you suddenly see a lot more floaters or notice big changes in their appearance, especially if they look like a shower of dark specks or a cobweb, it’s important to get your eyes checked.
- Persistent Flashes of Light: If you experience persistent or frequent flashes of light, especially in your side vision or along with a lot of floaters, it’s essential to tell an adult or visit an eye doctor.
- Loss of Side Vision or a Shadow in Your Vision: If you notice a curtain-like shadow or a loss of side vision, it could be a sign of a more severe problem like retinal detachment. In this case, seek immediate help.
What are the treatment options for Floaters and Flashes?
In most cases, floaters and occasional flashes don’t require treatment. However, if they’re affecting your vision significantly or are accompanied by other concerning symptoms, your eye doctor might suggest certain treatments or techniques.
Diabetic Retinopathy
What is Diabetic Retinopathy?

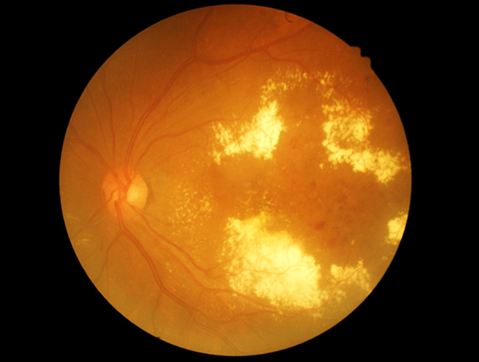
When tiny vessels in the back of the eye are damaged over a long period of time (usually > 7 years) in diabetic patients. This causes gradual build up of abnormalities in the retinal vasculature with vessels that at first leak fluid and protein and eventually start to bleed. If left untreated it will cause permanent vision reduction and even blindness.
What are the stages of Diabetic Retinopathy?
- Mild nonproliferativen diabetic retinopathy (NPDR)
- Moderate nonproliferative diabetic retinopathy
- Severe nonproliferative diabetic retinopathy
- Proliferative diabetic retinopathy (PDR)
Diabetic macula edema (DME) can occur in any of the stages of diabetic retinopathy and is caused by leaky blood vessels in the central part of the patients retina (macula). These cause fluid and lipid to leak out and will eventually cause permanent vision loss if left untreated.
Diabetic retinopathy is caused by gradual damage to the tiny vessels in the retina and reduced blood flow to some parts of the eye which in turn sends a signal for the eye to produce abnormal blood vessels which leak and bleed and lead to eventual vision loss.
How is Diabetic retinopathy diagnosed?
Through thorough eye examination that includes the following:
- Visual-acuity test
- Check of the intraocular pressure
- Slit lamp exam
- Dilated eye exam with check of the retina
- Fluorescein angiogram – a nontoxic dye test that is injected into a patients vein and when it travels to the eye the extent of the retinal abnormalities can be seen.
- Optical coherence tomography (OCT) – given doctors real time imaging of the retina and its structures in cross sectional view which allows to see swelling (edema) in the macula
What is the treatment of Diabetic Retinopathy?
- Diabetic macula edema (DME) in Mild/moderate/severe NPDR – treated traditionally with focal laser to close off leaking vessels however in the past 20 years there has been advent of medicines doctors inject in the eye of the patien (anti-VEGF medications). The original of such injectable medicine is Avastin but there are now multiple other options such as Lucentis, Eylea, Eylea HD, Cimerli, Byooviz and Vabysmo. As a group these are antibodies or antibody fragments which bind a growth factor in the eye and selectively shrink abnormal blood vessels. This treatment is often done on continuous basis with interval between injections chosen by your physician based on the response to the treatment. The other options for treatments included steroid injections such as Kenalog, Ozurdex and Illuvien. These have slightly more side effects but can be very effective at controlling DME for longer periods of time.
- Treatment of Proliferative Diabetic retinopathy involves injections with anti-VEGF agents similar to DME treatment as well as a more permanent treatment with panretinal laser photocoagulation (PRP). This procedure requires several treatment sessions and treats outside edges of the retina to shrink abnormal vessels which are often prone to hemorrhages. If not treated this will lead to permanent blindness due to a bleeding or retinal detachment. Close follow up is paramount in diabetic retinopathy. In more severe cases it is sometimes necessary to proceed with surgery called Pars Plana Vitrectomy.
- Reducing the risk of Diabetic Retinopathy
How can you reduce the risk of Diabetic Retinopathy?
A patient with diabetes should have an annual comprehensive dilated-eye exam. In the United States, more than 40 percent of diabetics have some form of diabetic retinopathy.
The risk of developing diabetic retinopathy can be minimized by doing the following:
- Monitoring changes in vision
- Keeping blood-glucose level low
- Monitoring and managing blood pressure
- Eating a healthy diet of low carbohydrates
- Participating in a regular exercise routine
- Monitoring and managing cholesterol levels
Patients with proliferative retinopathy can reduce their risk of blindness by 95% by keeping up with medical examinations, and promptly getting necessary treatment.
Uveitis
What is Uveitis?
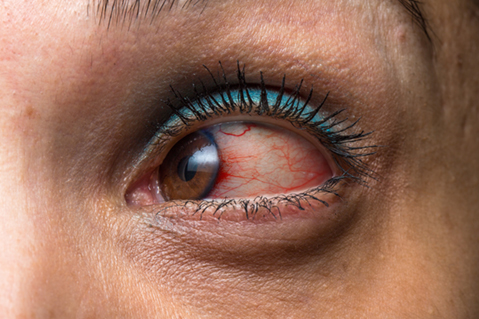
The uvea is the middle layer of the eye, consisting of the iris, ciliary body, and choroid. When this part becomes inflamed, it’s called uveitis. Inflammation can occur for various reasons, such as infections, injuries, or autoimmune diseases. Uveitis can affect one or both eyes and can be mild or severe.
What are the symptoms of Uveitis?
Uveitis can have different symptoms, and they might vary from person to person. Some common signs include:
- Eye Redness: The affected eye might appear red or bloodshot.
- Eye Pain: You might feel pain or discomfort in the affected eye, which can range from mild to severe.
- Blurry Vision: Your vision might become blurry or cloudy.
- Sensitivity to Light: You might feel more sensitive to light than usual.
- Floaters: Like small specks or shapes floating in your vision.
What are the types of Uveitis?
There are different types of uveitis depending on which part of the uvea is affected:
- Anterior Uveitis: This affects the front part of the eye, particularly the iris. It’s the most common type and is also known as iritis.
- Intermediate Uveitis: When the inflammation occurs in the middle part of the eye, particularly the ciliary body, it’s called intermediate uveitis.
- Posterior Uveitis: This affects the back part of the eye, mainly the choroid.
- Panuveitis: When inflammation occurs in all parts of the uvea, it’s called panuveitis.
What are the treatment options for Uveitis?

Treatment for uveitis depends on its cause and severity. It’s essential to consult an eye doctor (ophthalmologist) for proper diagnosis and treatment. Some common treatments include:
- Eye Drops: These might contain anti-inflammatory medication to reduce inflammation and control the condition.
- Oral Medications: In some cases, your doctor might prescribe oral medications like corticosteroids or other drugs to manage inflammation.
- Steroid Injections: For severe inflammation, injections of steroids might be given around or inside the eye.
- Surgery: In rare cases where other treatments aren’t effective or complications arise, surgery might be necessary.
Macular Hole
What is a Macular Hole?
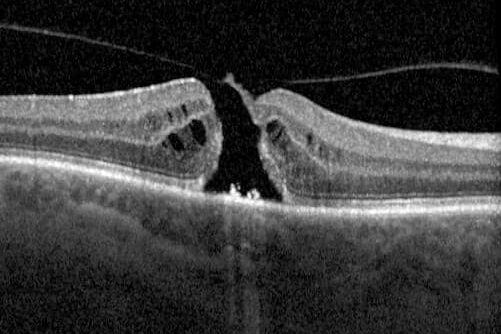
The macula is a tiny but essential part of the retina located at the back of your eye. It helps you see fine details clearly. A macular hole occurs when there’s a small break or opening in the macula, which can cause blurred or distorted vision.
What are the symptoms of a Macular Hole?
If you have a macular hole, you might experience the following symptoms:
- Blurry or Distorted Vision: Straight lines might appear wavy or bent. You might have difficulty reading or seeing details clearly.
- Central Blind Spot: You might notice a dark or blank spot in the center of your vision.
- Difficulty Recognizing Faces: People’s faces might seem blurry or distorted.
- Decreased Central Vision: Your ability to see things clearly in the center of your vision might diminish.
What causes a Macular Hole?
Most macular holes happen due to natural changes as people age. Other causes might include eye injuries, certain eye diseases, or rarely, long-term nearsightedness.
What are the treatment options for Macular Hole?
Fortunately, there are treatments available for macular holes, especially if detected early. Some common treatments include:
- Vitrectomy: This surgical procedure involves removing the vitreous gel inside your eye and replacing it with a special gas or oil bubble to help close the hole. Over time, the hole usually heals and closes.
- Face-Down Positioning: After surgery, you might need to keep your head face-down for some time to help the bubble push against the hole and promote healing.
- Medication: Your doctor might prescribe eye drops or other medications to prevent infection and help with healing after surgery.
